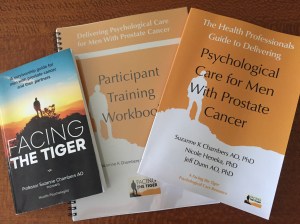
Facing the Tiger is a psychological care approach to improve the quality of prostate cancer survivorship by providing a manualized evidence-based solution for nurses and other health professionals supported by a patient self-support resource designed as a low intensity psychological intervention.
Worldwide, millions of men are living with a diagnosis of prostate cancer.
It’s tough living with that diagnosis. While the disease has one of the highest survival rates of any cancer, the side effects of treatment can be distressing, life-long and take a heavy toll.
Compared with the general population, men with prostate cancer are twice as likely to experience depression and three times more likely to experience anxiety. They have a 70% greater risk of suicide. Their distress is often hidden as many men are reluctant to ask for psychological help or admit to significant personal difficulties.
Research continues to show that men and the doctors, nurses and allied health professionals who look after them report the experience of prostate cancer treatment as challenging and uncoordinated. Survivorship care provision is fragmented, under-resourced, and often distressing for the patient. A man’s quality of life in prostate cancer survivorship remains poor for far too many.
Facing the Tiger helps nurses and other health professionals working with prostate cancer patients provide appropriate psychological support within their existing skill set and professional capabilities. It is an easy-to-implement yet powerful approach developed from decades of world-leading psycho-oncology research and practice by Professor Suzanne Chambers AO and colleagues. It is appropriate for use in a range of medical settings and does not require extra staff.
Facing the Tiger emphasises using the Australian-developed Psychosocial Care Model for Men with Prostate Cancer and the Prostate Cancer Survivorship Essentials Framework.
Here’s how it works.